From Pain to Perfect — We Care for Your Smile.
Alveolar Osteitis: The Complete Guide to Dry Socket Pain, Causes and Healing
Severity:
Teeth Problems:
If you've ever had a tooth extracted, you likely heard the term "dry socket" as a cautionary tale. But behind this common phrase lies a clinical reality with a more formal name: Alveolar Osteitis (AO). More than just a missing blood clot, this condition represents a profound disruption in your body's careful healing process, leading to pain that can feel overwhelming. Knowing its true name and nature is the first step in demystifying the experience and empowering your recovery.
The Many Names of a Shared Pain
When you're in pain, terminology might seem like the least of your concerns. However, the variety of names for this single condition reflects the medical community's long journey to understand it. Each term offers a different window into what's happening in your jaw:
-
Alveolar Osteitis (AO): The most precise clinical term. "Alveolar" refers to the tooth socket, "osteo" to bone, and "itis" to inflammation. It directly names the issue: inflammation of the bone within the socket.
-
Dry Socket: The common, visceral term we all know. It describes the hallmark sign dentists find: an empty, dry-looking socket where a protective blood clot should be.
-
Fibrinolytic Alveolitis: A term rooted in a leading theory. It suggests the condition is caused by the premature breakdown (fibrinolysis) of the vital blood clot.
-
Alveolalgia: Simply means "pain in the alveolus (socket)." A direct acknowledgment of your primary symptom.
-
Alveolitis Sicca Dolorosa: An older, almost poetic term meaning "painful, dry inflammation of the socket." It captures the full, distressing experience.
Not Just an "Infection": The True Nature of the Ache
A critical point of understanding—and often a source of confusion—is that Alveolar Osteitis is typically not a bacterial infection in its primary form. Think of it less like an invading army of germs and more like a construction site that has lost its essential blueprint and security.
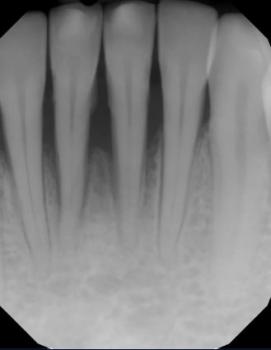
When your tooth is extracted, your body's first and most crucial job is to form a stable blood clot in the socket. This clot is not just a plug; it's a living scaffold. It protects the underlying bone and nerve endings from the outside world and serves as the foundation from which new tissue and bone will grow.
In Alveolar Osteitis, this scaffold disintegrates or washes away too soon. The result is that the exquisitely sensitive bone and nerve network at the base of the socket are left exposed to air, food, fluids, and temperature changes. This exposure triggers a significant localized inflammatory response—your body's alarm system going into overdrive in a very confined, vulnerable space. It is this inflammation of the bone itself that causes the severe, deep, and throbbing pain. While a secondary bacterial infection can complicate the picture later, the initial, intense pain is primarily from this inflammatory process.
The Emotional and Physical Toll: More Than Just a Toothache
To call the pain of a dry socket a mere "toothache" is a profound understatement. It is an experience that can dominate your entire being.
-
The Quality of Pain: Patients often describe it as a deep, throbbing ache that radiates up toward the ear, down the neck, or across the side of the face. It can feel like a heartbeat in your jawbone, a persistent pulse of distress that painkillers struggle to touch.
-
The Daily Disruption: This pain rewrites your daily life. It can turn simple joys—enjoying a meal, sipping a warm drink, laughing with a friend, or even finding a comfortable position to sleep—into sources of dread and discomfort. The constant, gnawing presence can lead to frustration, exhaustion, and a feeling of isolation.
-
The Cycle of Worry: It's common to spiral into questions: "Did I do something wrong?" "Is this normal?" "Why isn't it getting better?" This mental burden adds an emotional weight to the physical suffering.
Your Path to Relief: Why Professional Care is Non-Negotiable
If you recognize these signs—especially if severe pain emerges or intensifies 1 to 3 days after an extraction—it is crucial to understand that this is not a condition to "tough out." Home remedies may offer fleeting comfort but cannot address the core problem: the unprotected, inflamed socket.
Contacting your dentist or oral surgeon is an act of self-compassion, not a sign of failure. When you return to the clinic:
-
They will provide a definitive diagnosis, confirming it is Alveolar Osteitis and not another complication.
-
The treatment is focused and effective. They will gently cleanse the socket to remove any debris that is irritating the area.
-
They will then place a medicated dressing directly into the socket. This dressing serves a dual purpose: it delivers targeted pain-relieving and anti-inflammatory medication to the source of the pain, and it acts as a protective barrier, shielding the exposed bone to allow the healing process to restart properly.
The relief following this treatment is often swift and transformative. It allows your body, and your mind, to finally rest and truly begin to heal.
Remember: You are not just managing a "dry socket." You are healing from Alveolar Osteitis, a recognized inflammatory condition. By seeking professional care, you are not admitting defeat; you are taking the single most powerful step to reclaim your comfort and your peace. Allow your dental team to provide the relief and support you need. You deserve it.