Missing Teeth? Find Your Smile Again.
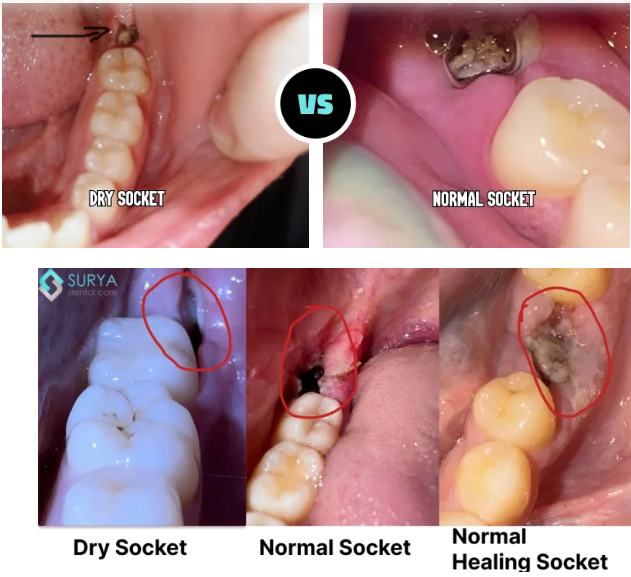
Dry Socket or Normal Healing? What to Expect After Tooth Extraction - Signs, Stages & When to See a Dentist
Severity:
Thanks — I looked closely at the photo. I can’t give a definitive medical diagnosis from a single photo, but I’ll walk you through what I can see, the differences between normal healing / dry socket / infection, what to watch for, typical timelines, what the dentist will do, how things can get worse if left, and immediate self-care + next steps.
Quick visual impression (from the photo)
-
The socket shows a dark area in the extraction site — that can be a blood clot or residual blood/debris.
-
I don’t clearly see obvious pus or gross swelling in this photograph, but the image is limited (lighting, angle, saliva and soft-tissue can hide signs).
-
Because the extraction was just yesterday, it is very early to tell: normal early healing often looks like a dark/blackish clot in the first 24–48 hours.
Complete Guide : Alveolar Osteitis: The Complete Guide to Dry Socket Pain, Causes and Healing
Other Topics: Implant vs Bridge which once is best for fast recovery
Key differences (what to expect and what signals dry socket or infection)
-
Normal early healing (first 1–3 days)
-
Pain should gradually decrease after the first 24–48 hours (mild–moderate discomfort controlled by OTC pain meds).
-
-
Dry socket (alveolar osteitis)
-
Usually starts 2–4 days after extraction.
-
Classic signs: severe, throbbing pain that radiates to the eye/ear, an empty-looking socket or exposed bone, bad taste/bad breath, pain increases rather than decreases.
-
Often the clot is lost or fails to form properly.
-
Stories and case dry socket:
- The Ache That Grew: A West Virginia Story of Dry Socket and Dental Regret
- Florida Dental Health Warning: Skipping Checkups Leads to Tooth Loss
- US Kentucky Dental Clinic Locator: Immediate Treatment for Dry Socket (Alveolar Osteitis)
-
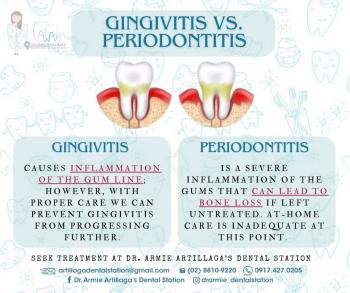
Infection (post-extraction infection)
-
-
Signs: increasing swelling, redness, pus or yellow/green discharge, fever, swollen lymph nodes, worsening pain after an initial improvement.
-
Infection can start any time but is more likely to show up a few days after extraction.
-
Given your history (previous dry sockets)
-
A history of previous dry sockets increases your risk. That means you should watch symptoms closely for the next 48–72 hours.
Immediate self-care (what to do now)
-
Do not aggressively rinse, spit, or use a straw for the first 24 hours. After 24 hours, gently rinse with warm salt water (½ teaspoon salt in 240 mL/8 oz warm water) 3–4× daily — gently, don’t force water into the socket.
-
Avoid smoking, vaping, or heavy physical exertion — these dislodge clots.
-
Cold compress for the first 24 hours (10–15 minutes on, 10–15 off) to reduce swelling/pain if present.
-
Pain control: ibuprofen (if you can take it) 400–600 mg every 6–8 hours as needed (follow label / healthcare advice); alternating with acetaminophen is common if needed.
-
Keep oral hygiene: brush other teeth gently; avoid direct brushing of the socket for a few days.
-
Soft diet; avoid hard/chewy foods that irritate the site.
When to see a dentist or go urgently
-
Go to emergency / dental urgent care immediately if you have: spreading facial swelling, fever (≥38°C/100.4°F), difficulty breathing or swallowing, uncontrolled bleeding, or rapidly worsening pain.
What your dentist will likely do
-
Clinical exam and possibly a gentle irrigation to remove debris.
-
If dry socket is suspected: they will usually clean the socket and place a medicated dressing (analgesic packing such as eugenol-soaked dressing) to reduce pain and protect the socket — re-dressings every few days until healing progresses.
-
If there are signs of infection: they may prescribe antibiotics (amoxicillin or similar) and/or drain/clean the socket.
-
Advice for follow-up and pain control.
Typical healing timelines
-
Clot forms/initial hemostasis: immediate–24 hours.
-
Pain peak: often first 24–72 hours; dry socket pain often worse around days 2–4.
-
Granulation tissue forms: ~3–7 days. Pain should significantly decrease by day 3–4 with normal healing or with treatment for dry socket.
-
Complete bone remodeling: months.
If everything goes normally, expect substantial improvement in 3–7 days and soft-tissue closure by 10–14 days. If it’s a dry socket and left untreated, pain may persist for a week or more; with treatment pain typically improves within a few days and socket heals within about 7–10 days.
What can scale up (potential complications if untreated)
-
Persistent severe pain (reduced quality of life, inability to eat/sleep).
-
Spread of infection → cellulitis or abscess (facial swelling, fever, systemic illness) — more serious and requires antibiotics and possibly hospitalization if severe.
-
Delayed healing of the socket; in rare cases osteomyelitis (bone infection) if infection spreads — much less common but serious.
-
Continued loss of nutrition / dehydration if pain prevents eating.
Practical next steps for you right now
-
Continue gentle salt-water rinses starting 24 hours after extraction.
-
Use recommended analgesics and avoid smoking or anything that disturbs the socket.
-
Call your extracting dentist or visit a clinic within 48–72 hours for a check — especially because you’ve had dry sockets before. Early professional treatment prevents prolonged pain.
-
If you want a local clinic, use your directory: https://cebudentalimplants.com/map-dental-clinic — search for the nearest open clinic and request a post-extraction check.
Final summary
-
From the photo alone (extraction yesterday) it most likely looks like a normal early clot — too soon to declare dry socket or infection.
-
Because you’ve had dry sockets in the past, be extra cautious and get an in-person check within 48–72 hours or sooner if pain worsens, foul taste develops, or you get fever/swelling.
-
If dry socket does develop (usually 2–4 days after extraction), your dentist can treat it quickly with a medicated dressing and you should feel better in a few days.
If you want, tell me: what tooth was taken out (upper/lower, wisdom or molar?), whether you’re smoking, and what pain level you have now (0–10) and if you have fever — I can tailor the advice a bit more.