Smile Again with Comfort and Confidence.
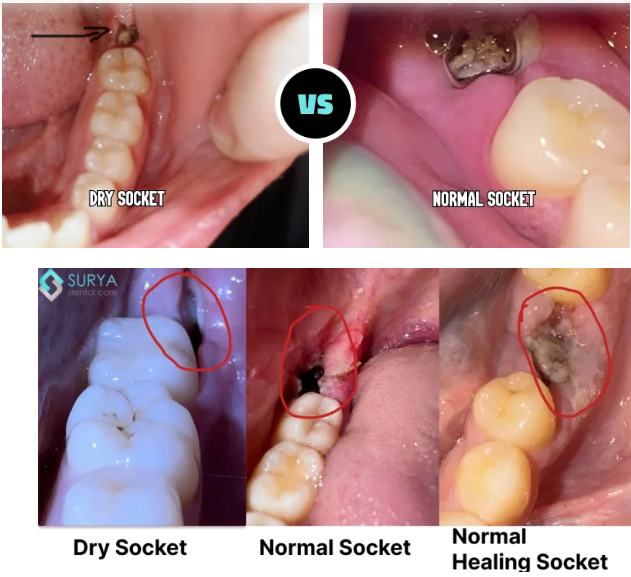
Dry Socket or Normal Healing? What to Expect After Tooth Extraction - Signs, Stages & When to See a Dentist
Severity:
Thanks — I looked closely at the photo. I can’t give a definitive medical diagnosis from a single photo, but I’ll walk you through what I can see, the differences between normal healing / dry socket / infection, what to watch for, typical timelines, what the dentist will do, how things can get worse if left, and immediate self-care + next steps.
Quick visual impression (from the photo)
-
The socket shows a dark area in the extraction site — that can be a blood clot or residual blood/debris.
-
I don’t clearly see obvious pus or gross swelling in this photograph, but the image is limited (lighting, angle, saliva and soft-tissue can hide signs).
-
Because the extraction was just yesterday, it is very early to tell: normal early healing often looks like a dark/blackish clot in the first 24–48 hours.
Complete Guide : Alveolar Osteitis: The Complete Guide to Dry Socket Pain, Causes and Healing
Other Topics:
Implant vs Bridge which once is best for fast recovery
bone-graft-vs-no-bone-graft-which-is-safer-dental-implant
dry-socket-symptoms-severe-pain-bad-smell-exposed-bone
Key differences (what to expect and what signals dry socket or infection)
-
Normal early healing (first 1–3 days)
-
Pain should gradually decrease after the first 24–48 hours (mild–moderate discomfort controlled by OTC pain meds).
-
-
Dry socket (alveolar osteitis)
-
Usually starts 2–4 days after extraction.
-
Classic signs: severe, throbbing pain that radiates to the eye/ear, an empty-looking socket or exposed bone, bad taste/bad breath, pain increases rather than decreases.
-
Often the clot is lost or fails to form properly.
-
Stories and case dry socket:
- The Ache That Grew: A West Virginia Story of Dry Socket and Dental Regret
- Florida Dental Health Warning: Skipping Checkups Leads to Tooth Loss
- US Kentucky Dental Clinic Locator: Immediate Treatment for Dry Socket (Alveolar Osteitis)
-
Infection (post-extraction infection)
-
-
Signs: increasing swelling, redness, pus or yellow/green discharge, fever, swollen lymph nodes, worsening pain after an initial improvement.
-
Infection can start any time but is more likely to show up a few days after extraction.
-
White Patch in Tooth Socket: Dry Socket or Normal Healing?
Many patients notice a white patch in the extraction site and immediately worry about infection.
In most cases, a white patch is granulation tissue — part of normal healing. It forms after the blood clot and protects the exposed bone.
However, if the white area is accompanied by severe throbbing pain or an empty-looking socket, it may indicate dry socket.
Pain level is the most important clue.
Why Your Tooth Socket Looks White Instead of Red
On Day 1, the socket appears dark red due to the blood clot.
By Day 2–4, the surface may turn white or cream-colored. This is a normal extraction wound look during the early healing stage.
The white appearance does not automatically mean pus.
Healing color progression:
• Dark red – blood clot
• White/cream – granulation tissue
• Pink – new gum forming
White Stuff in Wisdom Tooth Hole: Is It Different?
Wisdom tooth extractions leave larger, deeper sockets.
Because of this, white tissue may look more noticeable on Day 2–3. Mild swelling and jaw stiffness are common.
If pain improves daily, healing is normal.
If pain becomes sharp and spreads toward the ear, it may be dry socket.
Dry Socket Timeline: When Symptoms Usually Begin
Dry socket most commonly develops between Day 2 and Day 5 after extraction.
Warning signs include:
• Severe worsening pain
• Empty-looking socket
• Visible bone
• Strong bad breath
Normal healing discomfort improves daily. Dry socket pain intensifies.
Can Food Debris Look Like a White Patch?
Yes. Trapped food can resemble white tissue inside the socket.
Food debris may:
• Move when gently rinsed
• Appear chunky
• Cause mild bad taste
After 24 hours, rinse gently with warm salt water. Do not poke the socket.
Why Workers Who Return to Work Early Have Higher Dry Socket Risk
Returning to work too soon increases clot disturbance.
Workers who:
• Lift heavy objects
• Talk continuously
• Skip hydration
• Smoke during breaks
have a higher chance of dry socket between Day 2–5.
Protecting the clot protects your recovery.
When to See a Dentist Immediately
Seek dental care if you experience:
• Severe increasing pain
• Fever
• Thick yellow discharge
• Swelling after Day 3
• Pain radiating to ear or temple
Early treatment prevents longer healing time.
Given your history (previous dry sockets)
-
A history of previous dry sockets increases your risk. That means you should watch symptoms closely for the next 48–72 hours.
Immediate self-care (what to do now)
-
Do not aggressively rinse, spit, or use a straw for the first 24 hours. After 24 hours, gently rinse with warm salt water (½ teaspoon salt in 240 mL/8 oz warm water) 3–4× daily — gently, don’t force water into the socket.
-
Avoid smoking, vaping, or heavy physical exertion — these dislodge clots.
-
Cold compress for the first 24 hours (10–15 minutes on, 10–15 off) to reduce swelling/pain if present.
-
Pain control: ibuprofen (if you can take it) 400–600 mg every 6–8 hours as needed (follow label / healthcare advice); alternating with acetaminophen is common if needed.
-
Keep oral hygiene: brush other teeth gently; avoid direct brushing of the socket for a few days.
-
Soft diet; avoid hard/chewy foods that irritate the site.
When to see a dentist or go urgently
-
Go to emergency / dental urgent care immediately if you have: spreading facial swelling, fever (≥38°C/100.4°F), difficulty breathing or swallowing, uncontrolled bleeding, or rapidly worsening pain.
What your dentist will likely do
-
Clinical exam and possibly a gentle irrigation to remove debris.
-
If dry socket is suspected: they will usually clean the socket and place a medicated dressing (analgesic packing such as eugenol-soaked dressing) to reduce pain and protect the socket — re-dressings every few days until healing progresses.
-
If there are signs of infection: they may prescribe antibiotics (amoxicillin or similar) and/or drain/clean the socket.
-
Advice for follow-up and pain control.
Typical healing timelines
-
Clot forms/initial hemostasis: immediate–24 hours.
-
Pain peak: often first 24–72 hours; dry socket pain often worse around days 2–4.
-
Granulation tissue forms: ~3–7 days. Pain should significantly decrease by day 3–4 with normal healing or with treatment for dry socket.
-
Complete bone remodeling: months.
If everything goes normally, expect substantial improvement in 3–7 days and soft-tissue closure by 10–14 days. If it’s a dry socket and left untreated, pain may persist for a week or more; with treatment pain typically improves within a few days and socket heals within about 7–10 days.
What can scale up (potential complications if untreated)
-
Persistent severe pain (reduced quality of life, inability to eat/sleep).
-
Spread of infection → cellulitis or abscess (facial swelling, fever, systemic illness) — more serious and requires antibiotics and possibly hospitalization if severe.
-
Delayed healing of the socket; in rare cases osteomyelitis (bone infection) if infection spreads — much less common but serious.
-
Continued loss of nutrition / dehydration if pain prevents eating.
Practical next steps for you right now
-
Continue gentle salt-water rinses starting 24 hours after extraction.
-
Use recommended analgesics and avoid smoking or anything that disturbs the socket.
-
Call your extracting dentist or visit a clinic within 48–72 hours for a check — especially because you’ve had dry sockets before. Early professional treatment prevents prolonged pain.
-
If you want a local clinic, use your directory: https://cebudentalimplants.com/map-dental-clinic — search for the nearest open clinic and request a post-extraction check.
Final summary
-
From the photo alone (extraction yesterday) it most likely looks like a normal early clot — too soon to declare dry socket or infection.
-
Because you’ve had dry sockets in the past, be extra cautious and get an in-person check within 48–72 hours or sooner if pain worsens, foul taste develops, or you get fever/swelling.
-
If dry socket does develop (usually 2–4 days after extraction), your dentist can treat it quickly with a medicated dressing and you should feel better in a few days.
If you want, tell me: what tooth was taken out (upper/lower, wisdom or molar?), whether you’re smoking, and what pain level you have now (0–10) and if you have fever — I can tailor the advice a bit more.