Dentures That Feel Natural, Look Beautiful.
Optimizing Periapical Lesion Treatment: Step-by-Step Endodontic Protocol, Healing Timeline, and When to Act
Severity:
Teeth Problems:
Optimizing Periapical Lesion Treatment: Full Diagnosis, Endodontic Protocol, Healing Timeline, and Management Guide
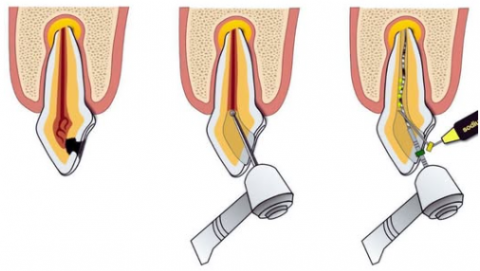
A periapical lesion is a radiolucent area at the tip of a tooth’s root, usually caused by pulp necrosis, infection, or chronic inflammatory breakdown of bone. Managing such a lesion requires accurate diagnosis, a step-by-step endodontic protocol, and a well-monitored healing timeline. The diagram provided visually represents the modern clinical sequence of removing infected pulp, shaping and disinfecting the canal, and sealing the root system to stop infection and allow bone regeneration.
This expanded guide explains the lesion, treatment sequence, expected healing within 14 days, red flags, and what happens if the condition is not treated promptly.
1. Full Analysis and Diagnosis
Radiographic Findings
A periapical radiolucency typically shows:
-
Breakdown of lamina dura
-
Dark circular or irregular area at the root apex
-
Loss of trabecular bone pattern
-
Widened periodontal ligament space
These findings usually indicate:
-
Chronic apical periodontitis
-
Periapical abscess
-
Apical granuloma
-
Periapical cyst (if size is large and well-defined)
Clinical Symptoms May Include
-
Tooth non-vital or unresponsive to vitality tests
-
Sensitivity to biting or chewing
-
Mild or intermittent swelling
-
Possible drainage through sinus tract
-
Bad taste if pus is present
Some cases remain completely asymptomatic — despite severe infection.
Main Cause
The root canal becomes infected due to:
-
Deep decay
-
Failed fillings
-
Cracked tooth
-
Trauma
-
Previously incomplete root canal
2. Understanding the Diagram: Step-by-Step Endodontic Process
Phase 1: Removal of Infected Pulp Tissue
The dentist accesses the inner pulp chamber and removes:
-
Necrotic tissue
-
Bacteria
-
Inflammatory exudate
This step stops the source of infection.
Phase 2: Cleaning, Shaping, and Disinfecting the Root Canal System
The canal is mechanically shaped and irrigated with disinfecting solutions.
Objectives include:
-
Eliminating bacteria
-
Removing smear layer
-
Creating proper taper for sealing
-
Preventing reinfection
Common irrigants:
-
Sodium hypochlorite
-
EDTA
-
Chlorhexidine
Phase 3: Filling and Sealing the Canal (Obturation)
After proper disinfection, the canal is sealed with:
-
Gutta-percha
-
Bioceramic sealer or resin-based sealer
This prevents reinfection and stabilizes the tooth.
3. Healing Timeline After Treatment
Days 1–14
-
Inflammation begins to subside
-
Pain decreases significantly
-
Socket and periapical tissues stabilize
-
No more drainage or swelling
-
X-ray changes are not visible yet
1–3 Months
-
Early bone regeneration begins
-
Radiolucent area may start to shrink
-
Patient usually becomes symptom-free
6–12 Months
-
50–90 percent of bone repair is expected
-
Radiographic healing becomes clearly visible
12–24 Months
-
Complete bone fill-in possible
-
Radiolucency may disappear entirely
4. If Healing Does Not Improve by Day 14
Signs that treatment may not be progressing properly include:
-
Persistent or worsening pain
-
Continued swelling
-
Development of sinus tract
-
Persistent bad taste or pus
-
Lesion remains the same size or enlarges
-
Warm or cold sensitivity returning in nearby teeth
-
Difficulty chewing
If these occur, the clinical steps may be required:
-
Re-treatment of the root canal
-
Additional disinfection and irrigation
-
Placement of intracanal medicaments like calcium hydroxide
-
Consider apicoectomy (root-end surgery)
-
Extraction if the tooth becomes non-restorable
5. Potential Complications if Untreated
A periapical lesion can progress into:
-
Chronic bone destruction
-
Periapical cyst formation
-
Acute flare-ups or abscess
-
Facial cellulitis
-
Spread of infection to neighboring teeth
-
Tooth mobility and eventual loss
-
Sinus tract formation
Timely treatment prevents these outcomes.
6. Recommended Patient Process to Follow
-
Schedule a complete dental examination with X-ray (periapical or CBCT).
-
Perform pulp vitality testing.
-
Begin root canal therapy as soon as diagnosed.
-
Use antibiotics only if swelling or systemic involvement is present.
-
Return for scheduled follow-ups at 3, 6, and 12 months.
-
Maintain excellent oral hygiene to support healing.
-
Monitor the tooth for changes in bite pressure or sensitivity.
7. Professional Comments
The diagram represents an ideal flow for treating periapical lesions through endodontic therapy. This is the gold standard approach when the tooth is structurally restorable. Bone regeneration begins once the source of infection is removed. Delays in treatment significantly increase the risk of bone loss and surgical intervention.
8. Clinic Locator Recommendation
Patients should visit their nearest dental clinic for proper diagnosis and treatment.
Use the directory here:
https://cebudentalimplants.com/map-dental-clinic