Healthy Teeth, Happy Life.
How Fast Caries Can Progress - From Filling to Root Canal in 5 Months
Severity:
Teeth Problems:
Nice clear radiographs — thanks. I’ll give a focused clinical/radiographic read, a 0–14 day action plan you can use now, likely definitive options, what will get worse if ignored, and short practical comments for the patient and clinician.
Radiographic diagnosis (concise)
-
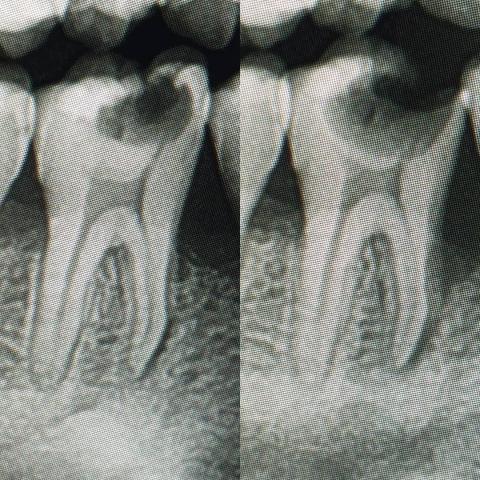
The images show a deep carious lesion extending into the pulpal chamber of a posterior tooth (likely a mandibular molar from the root morphology).
-
The caries appears to have progressed rapidly from enamel/dentin into the pulp; there is loss of coronal tooth structure and a widened pulp chamber outline consistent with pulpitis / pulpal involvement.
-
I do not see a large, well-defined periapical radiolucency in these images (no obvious chronic apical abscess), but early periapical changes can be subtle — pulp necrosis may already be present or developing.
-
Radiographic impression: Deep caries with probable irreversible pulpitis or early pulpal necrosis → endodontic treatment likely indicated. If the tooth is non-restorable clinically, extraction is the alternative.
Clinical tests to perform now (if you’re the treating dentist)
-
Vitality testing: cold test + EPT (compare adjacent teeth).
-
Percussion and palpation.
-
Periodontal probing to rule out vertical/root fracture or perio involvement.
-
Bite test to detect cracked-tooth pain.
-
Periapical radiograph(s) at different angulations; cone-beam (CBCT) only if planning complex retreatment or assessing root morphology.
-
Document symptoms: spontaneous pain, nocturnal pain, swelling, fistula, systemic signs.
Urgency & when to treat
-
If patient has swelling, fever, cellulitis or difficulty opening/ swallowing → emergency same-day care.
-
Otherwise: urgent — schedule endodontic evaluation/therapy within 3–7 days. Delaying longer (weeks–months) increases risk of abscess, spread, and possible tooth loss.
0–14 day practical care plan (what to do now)
Day 0–2 (triage):
-
Control pain: prescribe/advise appropriate analgesics (NSAID ± paracetamol per local dosing).
-
If there are systemic infection signs or rapidly spreading infection, start antibiotics (amoxicillin ± metronidazole) per guidelines — remember antibiotics do not treat pulpitis, only adjunct to spreading infection control.
-
If patient unable to attend immediate RCT and is symptomatic, consider emergency pulpotomy (if tooth is restorable and child/ adult cooperation allows) or placement of temporary medicated dressing to reduce symptoms.
Day 3–14 (definitive scheduling):
-
If coronal structure is insufficient for restoration, consider extraction and discuss space/successor tooth considerations (if applicable).
-
Following RCT: restore with a definitive coronal restoration; for posterior teeth consider a full coverage restoration (onlay/crown) to prevent fracture and re-infection.
Expected short-term results (14 days):
-
Pain and acute symptoms should markedly improve within 24–72 hours after appropriate endodontic therapy or emergency pulpal procedures.
-
Radiographic periapical healing requires months; absence of acute symptoms ≠ complete resolution of periapical radiolucency.
Definitive treatment options (short)
-
Pulpotomy/pulp therapy (only if reversible/partial pulpal involvement and indicated) — rare for adult permanent molars.
-
Conventional RCT → obturation → permanent coronal restoration (composite/onlay/crown).
-
Extraction when tooth is unrestorable or patient preference/financial constraints; discuss replacement options (implant, bridge, space maintainer if juvenile).
-
If complex anatomy or persistent symptoms → refer to endodontist (microscope/CBCT).
What will scale up if untreated
-
Progression to pulpal necrosis → acute apical abscess, sinus tract, cellulitis, possible systemic spread.
-
Increased treatment complexity and cost (from simple filling → RCT → possible extraction + prosthetic replacement).
-
Risk of tooth fracture when coronal tooth structure is weak.
-
Adjacent tooth/periodontium involvement or chronic infection impacting overall health.
Communication points to give the patient
-
“Delaying a small filling can allow bacteria to reach the nerve — that’s why what was a small appointment now needs RCT or extraction.”
-
RCT aims to remove infection and save the tooth; success rate is high but long-term success needs a good coronal seal/crown.
-
If pain/swelling develops — come back immediately.
Suggested workflow for clinician (concise)
-
Triage (phone/symptom check) → urgent appointment as needed.
-
Full clinical exam + pulp tests + periapicals (or CBCT if indicated).
-
If symptomatic reversible pulpitis: restore promptly. If irreversible pulpitis/necrosis: plan RCT or extraction.
-
Provide analgesia/antibiotics only when indicated.
-
Definitive restoration after endo within 1–4 weeks to prevent reinfection.
Short timelines summary
-
Emergency control (pain/infection): immediate (day 0–2).
-
Endodontic therapy scheduling: within 3–7 days ideally.
-
Symptom relief: often within 24–72 hours after RCT or proper pulpal procedure.
-
Radiographic periapical healing: 3–12 months depending on lesion size.
Local referral (your link)
For clinicians/patients in Cebu: use your clinic directory — https://cebudentalimplants.com/map-dental-clinic