Your Smile, Perfected with Precision.
Severe Tooth Decay and Gum Disease Linked to Diabetes – Life-Saving Dental Treatment in Cebu | Expert Care by Cebu Dental Implants Clinic
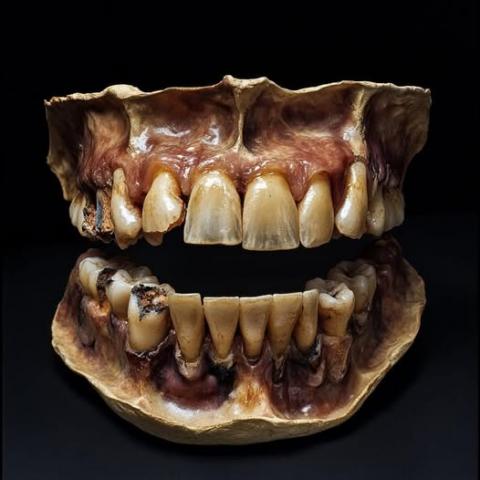
Severity:
Teeth Problems:
Image observations (zoom 100%)
-
Advanced generalized dental decay on multiple teeth (both arches). Dark cavitations and structural loss are evident.
-
Severe periodontal (gum) breakdown — gingival recession, exposed roots, inflamed/irregular gum margins.
-
Localized areas that look necrotic or grossly infected (dark, soft tissue changes near teeth).
-
Missing / broken teeth and heavy tissue destruction in posterior segments.
-
Overall poor oral environment — plaque/tooth debris and signs consistent with long-standing disease rather than a single acute cavity.
Probable diagnoses
-
Rampant caries (multiple teeth with deep decay)
-
Pulpitis and probable pulpal necrosis (teeth likely non-vital where cavities are deep)
-
Localized dental abscesses and chronic periodontal infection
-
Severe chronic periodontitis with bone loss (clinical picture fits advanced periodontal disease)
-
Systemic risk: potential for bacteremia from oral infection (important for diabetics, cardiac patients, immunocompromised)
Immediate risk level
High — there are signs of active, long-standing infection. If the patient has diabetes or any heart condition, the risk of systemic complications (endocarditis, poor glycemic control, sepsis) is significantly increased.
Urgent advice (today / 24–48 hours)
-
See a dentist or emergency dental clinic immediately. Do not wait if there is pain, swelling, fever, or difficulty swallowing.
-
If systemic symptoms (fever, facial swelling, rapid heartbeat, breathing difficulty) — seek emergency medical care.
-
Bring a list of current medications and any diabetes / heart disease history.
14-day treatment & recovery roadmap (realistic, best-case when care is available)
Day 0 (first visit)
-
Full clinical exam + periapical and panoramic X-rays to assess roots and bone.
-
If acute infection/abscess: start systemic antibiotics (per dentist/physician prescription) and analgesics.
-
Establish emergency plan: extraction vs endodontic treatment decisions for each tooth.
Days 1–3
-
Continue antibiotics and pain control.
-
Oral hygiene instruction + antiseptic mouth rinse (chlorhexidine if advised).
-
Referral for scaling/root planing if periodontal pockets amenable.
Days 4–7
-
Debridement and caries removal on restorable teeth; pulpotomy or root canal therapy for infected permanent teeth if salvageable.
-
Extractions for teeth non-restorable or severely infected. Simple extractions can be done promptly; surgical extractions may be scheduled.
-
Manage any soft tissue lesions (drainage of localized abscess if needed).
Days 8–14
-
Continued follow-up: check healing, suture removal (if any), and adjust treatment plan.
-
Begin definitive restorations for treated teeth (fillings, crowns) only when infection controlled.
-
If many teeth extracted, discuss interim prosthesis (partial denture) and long-term options (implants, bridges) once healed.
Expected outcome at 14 days (if compliant & no complications)
-
Significant reduction in pain and swelling.
-
Soft tissues healing; infection under control.
-
Definitive restorative work often requires more than 14 days (healing windows and lab work), but acute crisis should be managed.
If treatment is delayed 14 days or more, likely escalations
-
Spread of infection into facial spaces (cellulitis), deep neck infection, or risk of airway compromise.
-
Osteomyelitis (bone infection) of the jaw → longer course of antibiotics and surgery.
-
Sepsis or bacteremia → systemic organ risk, especially in diabetics or cardiac patients.
-
Worsening periodontal bone loss → tooth mobility and tooth loss.
-
Poorly controlled diabetes (if patient diabetic) — oral infection can impair glycemic control; conversely, high glucose worsens oral infection (vicious cycle).
-
Potential endocarditis risk in patients with certain heart conditions (requires medical coordination).
Practical patient instructions (what the patient can do now)
-
Take prescribed antibiotics exactly as directed; do not stop early even if pain improves.
-
Use recommended analgesics and a soft diet.
-
Rinse gently with warm saline or antiseptic rinse (per dentist).
-
Maintain gentle oral hygiene — soft toothbrush, avoid traumatizing inflamed tissue.
-
Monitor for fever, increasing swelling, spreading redness, difficulty breathing or swallowing — go to ER if any appear.
Comments for clinicians / notes to add in case record
-
Record systemic history: diabetes, heart disease, immunosuppression, medications (especially anticoagulants or cardiac meds).
-
Obtain radiographs and chart mobility/pocket depths.
-
Coordinate with patient's physician if diabetic or cardiac — may require antibiotic prophylaxis or blood sugar optimization.
Call to action — where to go
Find a trusted clinic near you and book an emergency consult:
https://cebudentalimplants.com/map-dental-clinic
(If the patient is in the Philippines and has diabetes or heart disease, advise contacting both a dentist and their physician immediately.)
comment
This image shows severe, long-standing oral disease with a high risk of active infection. Immediate dental assessment and treatment are essential. With rapid care, much of the acute pain and infection can be controlled within 7–14 days, but definitive rehabilitation (restorations, implants) will require longer follow-up. Delay increases risks to both oral and overall health — especially for diabetic or cardiac patients.