Your Smile, Perfected with Precision.
Post-Extraction Swelling & Bruising - Is It Dry Socket or Normal Healing?
Severity:
Teeth Problems:
Quick summary of the situation you described
-
Tooth was extracted 2 days ago.
-
Swelling started before extraction and has not gone down since.
-
Area is now bruised. Extraction was difficult/traumatic.
-
You did not take antibiotics (previous C. difficile).
-
You cannot take typical OTC pain meds (alpha-gal + stomach issues).
-
You avoided smoking, sucking straws, and brushing the site.
Possible diagnoses (differential)
-
Normal post-op inflammation/hematoma from a traumatic extraction
-
A difficult extraction often causes local soft-tissue bruising and swelling that can persist for several days. Bruising is consistent with tissue/soft-tissue trauma. Pain usually decreases gradually over 2–7 days.
-
-
Alveolar osteitis (dry socket)
-
Typical timing: 2–4 days after extraction. Classic signs: severe, throbbing pain radiating to ear/temple, an empty-looking socket with exposed bone, foul taste/odor, and lack of normal improvement. Dry sockets usually present with increased pain (not decreased) starting ~48–72 hours post-op. Swelling is less typical or mild.
-
-
Post-extraction infection / abscess
-
Signs include increasing swelling, redness, fever, spreading facial swelling, worsening pain, pus/drainage, or systemic symptoms. Infection risk is greater after a traumatic extraction but antibiotics are not always indicated unless clinical infection is present.
-
-
Hematoma
-
Localized collection of blood can cause persistent swelling and bruising; pain may be present but often less severe than dry socket.
-
Which is most likely here?
-
Because swelling and bruising were present before and persisted, and extraction was difficult, post-op inflammation/hematoma from trauma is a strong possibility.
-
If your pain is worse now than immediately after extraction (especially severe, radiating pain 48–72 hours after), dry socket becomes more likely.
-
Infection is possible if swelling is increasing, you have fever, spreading redness, or purulent drainage.
I cannot give a definitive diagnosis without seeing the socket (photo/clinical exam), but your history raises concern for either traumatic healing (hematoma/bruising) or early dry socket — so you should have the socket rechecked soon.
What to check (examination checklist for your dentist or for photos you can send them)
-
Is there an empty-looking socket with exposed pale bone?
-
Is there foul odor or pus/greyish discharge?
-
Is the pain worsening or radiating toward the ear/temple?
-
Is swelling increasing day-to-day or spreading to neck/eye area?
-
Any fever or difficulty breathing/swallowing?
If possible, take a close, well-lit photo (without probing) and send to your dentist.
Immediate home care you can safely try (since many meds are not an option)
Do these unless your dentist instructs otherwise:
-
Warm saline rinses (starting 24 hours after extraction):
-
Mix 1/2–1 tsp salt in 8 oz (240 mL) warm water; gently rinse 4–6×/day and after meals. This helps remove debris and reduces bacterial load.
-
-
Cold then warm compresses:
-
First 24–48 hours: apply cold pack to the outside of the cheek 10–20 minutes ON, 10 minutes OFF to reduce swelling.
-
After 48 hours: switch to warm compresses to encourage drainage/healing.
-
-
Keep head elevated while resting to reduce swelling.
-
Soft diet and avoid chewing on the side of the extraction.
-
Avoid vigorous rinsing, spitting, or puckering, but gentle saline is okay.
-
Topical measures: some people get temporary relief from a cotton pellet soaked in clove oil (eugenol) applied briefly to the socket — but this can irritate soft tissues and may contain allergens. Because you have alpha-gal and medication sensitivities, check with your dentist or physician before topical agents.
-
Oral hygiene: continue gentle brushing of other teeth; avoid direct brushing of the socket until advised.
-
If you have a medicated dressing at the clinic (e.g., Alvogyl) — return to your dentist to have it placed/changed. These dressings relieve pain quickly and protect the socket while it heals.
Important: Because you cannot take common oral analgesics, discuss alternatives promptly with your dentist/physician (see below).
Pain control alternatives & medication notes (you must check safety with your MD/dentist)
-
Acetaminophen (paracetamol) is often used if tolerated. You didn’t explicitly say you can’t take acetaminophen — if you can, it may help. Confirm with your physician.
-
If acetaminophen is not tolerated, a dentist may use local measures (medicated packing, local anesthetic gel) or, rarely, prescribe an alternative analgesic appropriate to your allergies/medical history. Don’t take antibiotics or analgesics without professional guidance given your CDI and alpha-gal issues.
-
Because of your past C. difficile, antibiotics should only be used if there is clinical infection — not as routine prophylaxis.
Timeline — what to expect
-
0–48 hours: peak swelling/pain from extraction and trauma; bruising visible.
-
48–72 hours: pain should start to improve. If pain worsens at 48–72 hours, think dry socket.
-
3–7 days: most traumatic swelling and pain decrease substantially. Socket begins granulation tissue formation.
-
7–14 days: most sockets show clear healing; residual discomfort usually minimal.
-
If symptoms persist or worsen at 10–14 days, consider complications: persistent dry socket, secondary infection, retained root fragment, or (rare) osteomyelitis — these require definitive assessment.
So if by day 7 you haven’t improved or if pain is worsening now (day 2 → day 3), contact your dentist urgently.
If it takes 14 days — what could scale up (possible complications)
-
Persistent alveolar osteitis (dry socket) causing prolonged severe pain and delayed healing.
-
Secondary infection / abscess — may require drainage and antibiotics (but antibiotics must be carefully chosen because of CDI history).
-
Retained root or sequestrum (dead bone) — may cause ongoing pain and require surgical removal.
-
Osteomyelitis (rare) — serious infection of the jaw bone; signs: severe pain, spreading swelling, fever, numbness; needs urgent care.
-
Delayed soft-tissue healing in smokers or with systemic problems (diabetes, immunosuppression).
If any spreading swelling, fever, difficulty breathing/swallowing, or rapidly worsening pain occurs at any time → seek emergency care immediately.
Practical immediate next steps (actionable)
-
Call your dentist today and describe: extraction was difficult, swelling present before procedure, now bruised and pain not improving 2 days after. Ask for urgent recheck or advice.
-
If you cannot see your dentist promptly, visit an urgent dental clinic or ER if you have worsening pain, fever, spreading swelling, or trouble breathing/swallowing.
-
Ask your dentist about placing a medicated dressing (pain relief and protection) in the socket — often provides quick relief for dry socket and is standard management.
-
Discuss pain medication alternatives with your dentist and your physician (safe choices given alpha-gal and prior C. diff).
-
Use the directory you provided to find a nearby clinic: https://cebudentalimplants.com/map-dental-clinic
Red flags — go to ER or call dentist immediately if:
-
Fever > 38°C (100.4°F) or rigors.
-
Rapidly spreading facial/neck swelling, difficulty breathing, or swallowing.
-
Severe, uncontrolled pain despite home measures.
-
Bleeding that won’t stop after gentle pressure for 20–30 min.
-
Numbness/tingling spreading beyond the local area.
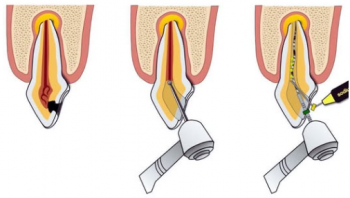
Examination & treatment your dentist may perform
-
Visual inspection and gentle irrigation of the socket.
-
Remove debris and place medicated dressing/paste (e.g., eugenol-containing dressing) for pain control.
-
If infection is present, they may take radiographs and consider appropriate antibiotic therapy (balancing CDI risk) — sometimes topical care + drainage suffices.
-
If retained root fragment or necrotic bone suspected, surgical management may be needed.