Smile Again with Comfort and Confidence.
The End of the Drill: How a Microneedle Patch is Revolutionizing Tooth Regeneration
Language :
Topics:
The End of the Drill? A Deep Dive into the Microneedle Patch Revolutionizing Tooth Regeneration
For centuries, dentistry has been defined by a single, dreaded sound: the whir of the drill. Its purpose is subtractive—to remove decayed matter before filling the void with artificial materials. But a groundbreaking discovery from researchers in South Korea is poised to flip this paradigm on its head, moving from a philosophy of replacement to one of regeneration.
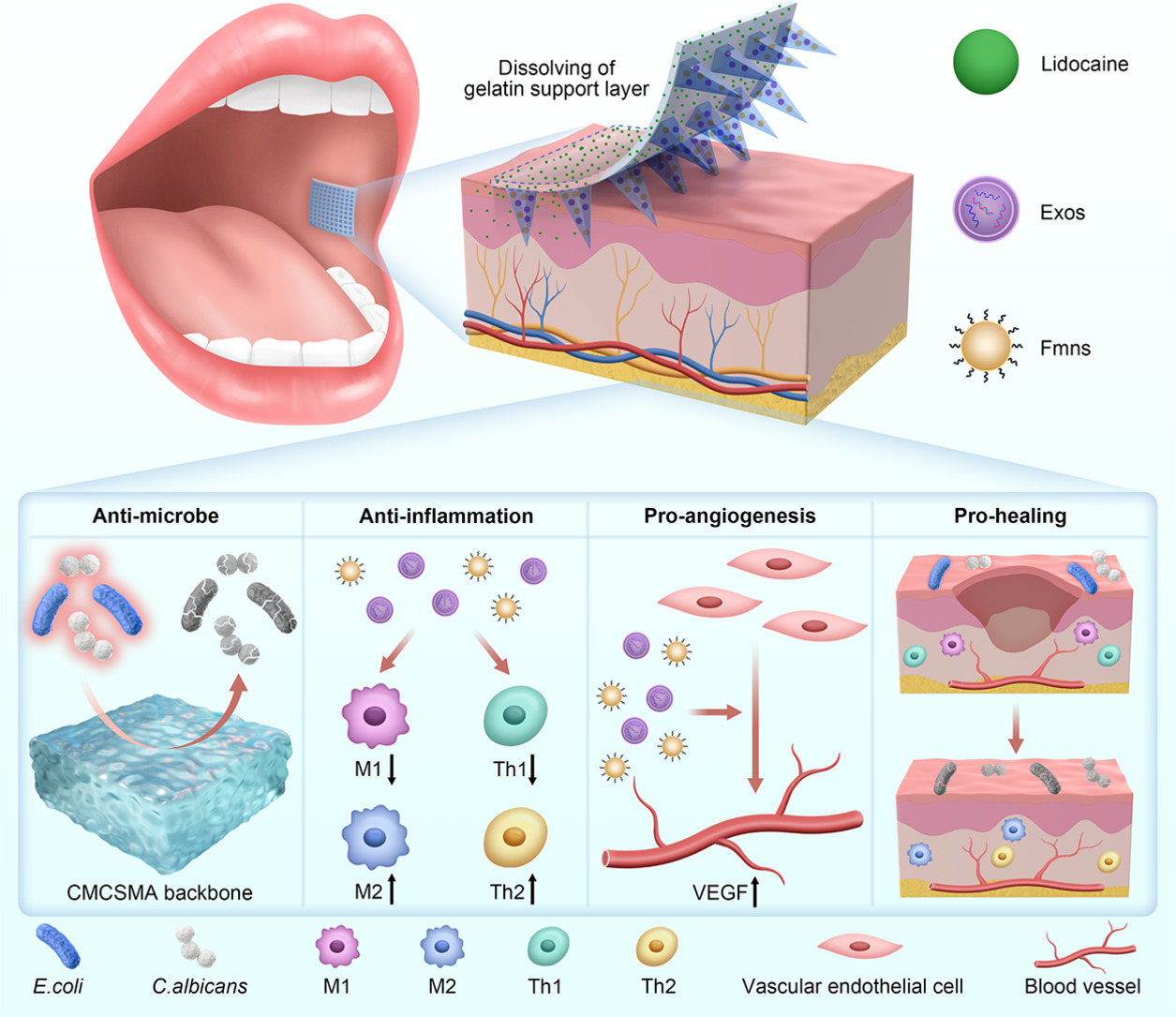
Expanding the Source: How the "Smart Microneedle Patch" Actually Works
The initial report can be summarized as a patch that regrows enamel. The reality is far more sophisticated and represents a convergence of biotechnology, material science, and stem cell therapy.
The system, developed by a team likely building on work from institutions like the Korea Advanced Institute of Science and Technology (KAIST) or Seoul National University, is a targeted drug delivery platform designed to activate the body's own repair mechanisms. Here's a detailed breakdown:
-
The Patch Structure: It's not a simple bandage. It's a two-part system:
-
Microneedles: These are tiny, biodegradable needles made from a substance like hyaluronic acid or a similar polymer. They are painlessly and precisely long enough to penetrate the non-sensitive enamel surface or reach the area around a tooth's root, but not deep enough to cause significant pain.
-
Therapeutic Cargo: The microneedles are loaded with bioactive molecules. The key ingredients are likely:
-
Stem Cell Mobilizers: Small molecules or growth factors (e.g., TGF-β, BMPs) that specifically target and activate dental pulp stem cells (DPSCs) and stem cells from the apical papilla (SCAP). These are the body's resident tooth-repair cells, typically dormant in adults.
-
Mineralization Promoters: Compounds that encourage the deposition of hydroxyapatite crystals, the primary mineral component of enamel and dentin.
-
-
-
The Regenerative Process:
-
Application: The patch is applied directly to the damaged area—be it an early cavity, a cracked surface, or even the socket of a lost tooth.
-
Delivery: The microneedles dissolve upon contact with moisture, releasing their cargo precisely where it's needed.
-
Activation: The released molecules diffuse into the tooth structure, signaling the nearby stem cells to "wake up," proliferate, and differentiate into ameloblasts (enamel-forming cells) or odontoblasts (dentin-forming cells).
-
Regeneration: These newly activated cells begin secreting the natural matrices of the tooth, effectively regenerating genuine, living enamel and dentin from the inside out. In the case of a lost tooth, the goal is to orchestrate the formation of a complete "tooth bud," recapitulating the natural process of tooth development.
-
Analysis of New Research and Future Directions
This breakthrough sits at the forefront of several converging fields. To understand its potential, we must look at the research it enables:
-
Overcoming the "Non-Renewable" Enigma: Mature enamel cannot regenerate naturally because the ameloblast cells die off after the tooth erupts. This technology bypasses that by either re-activating progenitor cells or guiding other stem cells to take on an ameloblast-like function. Future research will focus on ensuring the quality and long-term stability of this newly formed enamel, matching the incredible density of natural enamel.
-
The Race for the Perfect Biomolecule Cocktail: The specific combination of growth factors is the "secret sauce." Competing research labs and biotech startups are now racing to identify the most efficient, safe, and cost-effective cocktail. We will see studies comparing different factors and their ratios for optimal regeneration speed and structural integrity.
-
Integration with Digital Dentistry: The next logical step is to combine this biologic treatment with digital scans. A dentist could take a 3D scan of a cavity, and a printer could create a custom-fit microneedle patch that perfectly contours to the exact shape and depth of the lesion.
-
Addressing Complexities of Whole-Tooth Regeneration: Growing a simple layer of enamel is one thing; growing an entire, anatomically correct tooth with a pulp, nerves, and blood vessels is another. This requires the simultaneous regeneration of multiple tissue types (a field known as whole-tooth tissue engineering). The patch would need a scaffold to guide the growth and a more complex cocktail of molecules. This remains a longer-term goal, but the microneedle platform provides a viable delivery vehicle for it.
From Lab Bench to Global Scale: Revolutionizing the Worldwide Dental System
The transition from a successful lab prototype to a global standard of care is a monumental challenge. Here is how this discovery could scale massively:
Phase 1: Clinical Validation and Regulatory Approval (Next 5-8 Years)
-
Human Trials: Following successful animal studies, large-scale human clinical trials will be essential to prove efficacy and safety.
-
Regulatory Pathways: The patch will be classified as a combination product (device + biologic) requiring approval from bodies like the FDA (USA), EMA (Europe), and their global counterparts. A clear pathway will need to be established.
-
Initial Niche Applications: It will first be used for minimally invasive procedures—treating early-stage cavities (replacing the "watch and wait" approach), repairing cracked tooth syndrome, and desensitizing exposed roots.
Phase 2: Integration and Democratization (Next 8-15 Years)
-
Manufacturing Scale-Up: Producing millions of sterile, reliable patches requires advanced, automated manufacturing facilities. This will drive costs down through economies of scale.
-
Dental Professional Training: Dentists and hygienists will need new training. The skill set shifts from mechanical drilling to biological diagnosis and application. This could simplify certain procedures, making them accessible in a wider range of clinical settings, including public health clinics.
-
Reimbursement Models: Insurance companies and national health systems will need to create new billing codes and reimbursement structures for "biologic enamel regeneration" and "tissue engineering procedures."
Phase 3: Mass Adoption and System-Wide Transformation (15+ Years)
This is where the true disruption occurs, leading to a new dental ecosystem:
-
The Demise of the "Drill and Fill": The majority of simple fillings (amalgam, composite) become obsolete. The focus shifts from repair to regeneration. The psychological impact is huge—dentistry is no longer scary.
-
Preventive and Minimally Invasive Dentistry Becomes King: The patch makes it feasible to treat micro-cavities the moment they are detected, preventing them from ever becoming major issues. This aligns perfectly with the core philosophy of modern dentistry.
-
Addressing the Global Burden of Dental Disease: Dental caries is the most common non-communicable disease worldwide. A low-cost, easy-to-apply patch could be deployed in underserved and rural areas by community health workers, dramatically reducing global oral health disparities.
-
The Beginning of the End for Dentures and Implants? The long-term vision is to use this technology to regrow natural teeth. While implants are an excellent solution, they lack the periodontal ligament—the shock absorber of a natural tooth. A regenerated tooth would be a true biological replacement, superior to any current prosthetic. This would dismantle the multi-billion-dollar denture and implant industry as we know it, replacing it with a regenerative one.
-
Economic Impact: While it may reduce revenue from repetitive filling replacements, it will create massive new markets in biotechnology, advanced manufacturing, and digital health. It will also have a significant positive economic impact by reducing productivity loss due to dental pain and complex procedures.
Conclusion: A Paradigm Shift is Inevitable
The South Korean microneedle patch is more than a new product; it is the herald of a new era. It represents a fundamental shift from our current, mechanical intervention to a future where we harness the body's innate power to heal itself.
The path to scaling is complex, fraught with scientific, regulatory, and economic hurdles. Yet, the potential to eliminate the fear of the dentist's chair, to provide biologically perfect repairs, and to make tooth loss a reversible condition is a powerful motivator. The drill's days may not be numbered yet, but for the first time in history, we can hear the countdown beginning.
















