Transforming Smiles, Restoring Confidence.
Core Concept: Cavities Are Active Infections, Not Just Holes
Language :

Your statement is 100% correct. A cavity (dental caries) is a bacterial infection of the tooth structure. It begins when acids produced by bacteria in plaque demineralize (dissolve) the hard, outer enamel. This is the initial, often invisible, stage.
Once the enamel is breached, the infection progresses to the softer, more sensitive layer beneath it: dentin. Dentin is much less resistant to acid. From here, the infection can spread rapidly and in ways that are not always visible from the surface.
Detailed Topic Breakdown
1. The "Spreading" Nature of Cavities: How One Tooth Can Harm Its Neighbors
This is a crucial and dangerous aspect of untreated cavities.
-
Direct Surface Spread: The cavity expands within the tooth, destroying enamel and dentin. What starts as a tiny pit can undermine the entire tooth structure from the inside.
-
Interproximal Spread (Tooth-to-Tooth): Cavities frequently occur between teeth where cleaning is difficult. As the cavity grows on the side of one tooth, it creates a larger hidden space where plaque and bacteria accumulate, directly attacking the adjacent tooth. One cavity can indeed lead to two.
-
The Role of Bacteria: Your mouth is an ecosystem. A large, active cavity acts as a reservoir for high levels of destructive bacteria. These bacteria can be transmitted through saliva, increasing the overall bacterial load in your mouth and raising the risk for new cavities on other teeth, especially if they have pits, fissures, or existing weak spots.
2. The Signs of a Severe Infection: Smell and Black Color
The symptoms you described are classic indicators of advanced decay.
-
Intense Smell (Halitosis): The smell comes from two primary sources:
-
Bacterial Waste: The bacteria metabolizing food particles (especially sugars and proteins) in the cavity release volatile sulfur compounds (VSCs). These are the same compounds that give rotten eggs their smell and are a primary cause of bad breath.
-
Necrotic Tissue: As the cavity deepens and reaches the inner pulp (the living part of the tooth containing nerves and blood vessels), it causes pulpitis (inflammation) and eventually pulp necrosis (death). The dead tissue inside the tooth decomposes, producing a very potent and foul odor that brushing or mints cannot eliminate.
-
-
Black Color: The color change tells a story of progression:
-
White/Yellowish-Brown Spots: Early demineralization.
-
Light to Dark Brown: Active decay progressing through the enamel and dentin.
-
Black or Very Dark Brown: This often indicates that the decay has advanced significantly. The black color can be a sign of necrosis (dead tooth structure) or a long-standing, possibly slower-growing lesion where the dentin has been stained over time by bacterial byproducts and food pigments. A black cavity is almost always a deep cavity.
-
3. The Domino Effect: "Swallowing Your Teeth" and Harming Many Teeth
An untreated cavity doesn't stop. It follows a destructive path:
-
Enamel Penetration: Infection breaches the outer shell.
-
Dentin Destruction: Infection spreads rapidly underneath the enamel, potentially causing a large cavity hidden by a seemingly intact surface. The tooth may break during eating.
-
Pulp Invasion: Bacteria reach the nerve. This causes a severe toothache (but pain can subside once the nerve dies).
-
Root Canal Infection & Abscess: The infection travels through the root canals and out the tip of the root into the jawbone, forming a dental abscess (a pus-filled pocket). This is a serious infection that can cause swelling, fever, and intense pain.
-
Tooth Loss: The destruction can become so extensive that the tooth cannot be saved and must be extracted. This is the literal "swallowing of your teeth" – losing them.
-
Bone Loss: The abscess destroys the bone that holds the tooth in place. This bone loss can weaken the support for the adjacent teeth.
-
Systemic Health Risks: The bacteria from a dental abscess can enter the bloodstream (a condition called bacteremia), potentially leading to infections in other parts of the body (heart, sinuses, etc.), posing a risk to overall health.
Prevention: Breaking the Chain of Infection
Understanding that cavities are infections underscores the importance of prevention.
-
Mechanical Plaque Removal:
-
Brushing: Twice daily with fluoride toothpaste. Fluoride helps remineralize early lesions and strengthens enamel against acid.
-
Flossing: Non-negotiable. This cleans the interproximal surfaces where cavities often start and spread between teeth.
-
-
Dietary Control:
-
Limit the frequency of sugary and acidic foods/drinks. It's not just the amount, but how often your teeth are exposed to acid. Constant snacking or sipping soda fuels the bacteria all day.
-
-
Saliva: Saliva is your mouth's natural defense. It neutralizes acids, washes away food particles, and contains minerals for remineralization. Stay hydrated.
-
Professional Care:
-
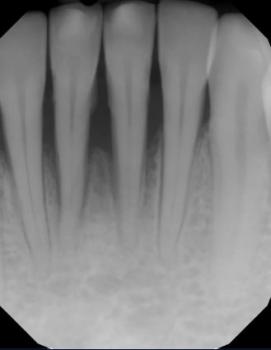
Regular Check-ups & Cleanings: Dentists and hygienists can remove hardened plaque (tartar) that you can't, identify early cavities (often with X-rays before they are visible), and provide professional fluoride treatments.
-
Sealants: A protective plastic coating applied to the chewing surfaces of back teeth to prevent decay in the deep grooves.
-
Your observation is the key to changing how we think about dental care. Viewing a cavity as a "harmless hole" is a dangerous misconception. It is, in fact, a dynamic bacterial infection that will spread, cause symptoms like bad smell and discoloration, and if left unchecked, will destroy the tooth, compromise neighboring teeth, and potentially affect your overall health. Proactive, consistent oral hygiene is not just about a bright smile; it's about actively preventing and controlling a chronic infectious disease.