Because Every Tooth Deserves Care.
Tooth Hurts When Biting? Signs of Hidden Infection or Failed Dental Filling
Severity:
Teeth Problems:
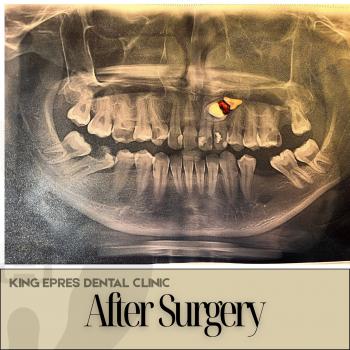
Immediate observations (zoomed image review)
-A metallic structure is visible on the lower posterior tooth area (looks like a crown/abutment or large restoration).
-The occlusal surfaces of adjacent molars show brown staining and pits consistent with caries (decay).
-The local gum tissue is mildly red and slightly swollen near the affected tooth — a sign of inflammation.
-No large facial swelling is obvious in the image, but the tissue around the tooth looks tender when manipulated (you reported pain).
Most likely causes of the pain (ranked)
-
Deep caries reaching the pulp → acute pulpitis (tooth nerve inflammation) — very common cause of severe tooth pain.
-
Failed/ leaking restoration or crown (the metal visible) allowing bacteria to enter under it → reinfection of the tooth or root.
-
Periapical abscess (infection at the root tip) beginning to form — often causes continuous pain and tenderness.
-
Cracked tooth / vertical fracture — can cause sharp pain on biting and persistent discomfort.
-
Localized gingival infection / food impaction exacerbating the pain.
Tests the dentist will do (next visit)
-
Periapical X-ray (or CBCT if available) to see root and bone involvement.
-
Pulp vitality tests (cold/electric) to check nerve status.
-
Percussion and bite tests to localize the painful tooth.
-
Clinical inspection for cracks and a probe for periodontal pockets.
Best immediate actions you can take (home care)
-
Avoid chewing on that side.
-
Rinse gently with warm salt water (1 tsp salt / cup warm water) 3× daily.
-
Over-the-counter analgesics: ibuprofen (if tolerated) or paracetamol/acetaminophen for pain control — follow dosing on the pack or your doctor’s advice.
-
Do not try to remove or pry at the restoration yourself.
-
If you have a dentist’s phone number, call for an urgent appointment.
Definitive clinical solutions (likely)
-
If pulp is infected but tooth restorable → Root canal treatment (RCT) followed by a new crown.
-
If the restoration/crown is failing → remove/replace the crown and assess underlying tooth; RCT if pulp involvement.
-
If tooth is non-restorable or fractured → extraction followed by socket management and options for replacement (bridge/implant) later.
-
If abscess present → drainage + antibiotics (antibiotics only if systemic signs or spreading infection; dentist will decide type/dose).
-
Occlusal adjustment if bite is stressing the tooth.
Typical healing / timeframes
-
Pain relief with analgesics: hours (temporary).
-
Symptom improvement after drainage/antibiotic (if needed): 24–72 hours.
-
Root canal completion & initial recovery: 1–2 weeks to feel much better; full comfort may take several weeks.
-
Extraction soft-tissue healing: 1–2 weeks (bone remodels over months).
-
If a crown/definitive restoration is placed: allow 1–2 weeks after final cementation for full comfort.
If NOT treated within 14 days — likely progression
-
Pain will often increase and become constant.
-
Local infection can progress to a dental abscess with pus, swelling, and bad taste/odor.
-
Infection can spread to adjacent teeth and bone (osteomyelitis) or cause a significant facial swelling.
-
Increased risk of tooth loss, more complex surgery, and longer healing times.
-
Rare but serious: spread of infection beyond oral tissues (seek emergency care for facial swelling, fever, breathing or swallowing difficulties).
Urgent warning signs — get immediate care if you have:
-
Increasing facial swelling or rapidly spreading redness
-
Fever, difficulty breathing or swallowing
-
Severe uncontrolled pain or inability to open mouth
Practical next steps (recommended)
-
Call and book an urgent dental appointment today.
-
Ask the clinic to take an X-ray and prioritize a possible endodontic (root canal) exam.
-
Follow home-care measures until you are seen.
Find a nearby clinic here:
https://cebudentalimplants.com/map-dental-clinic
Comment
This looks like a tooth that needs professional attention soon — most likely deep decay or a failing restoration with pulp involvement. Acting within the next few days to a week greatly increases the chance of saving the tooth with a root canal and new crown, and avoids an abscess or extraction. If you want, I can draft a short message you can send to a clinic to book an “urgent exam + X-ray” — ready to paste in the clinic’s contact form.