Missing Teeth? Find Your Smile Again.
Tooth Extraction Healing: What to Expect in 14 Days Signs of Infection, Pain Timeline, and When to See Your Dentist
Severity:
Teeth Problems:
Quick impression (based on the photo + your description)
-
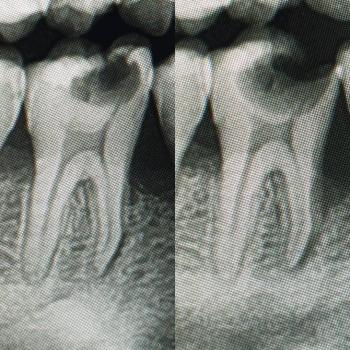
The socket area looks inflamed (red) with some pale/granulation-looking tissue inside the extraction site.
-
I cannot confirm infection, exposed bone, or dry socket for sure from a single photo — those need an in-person exam and maybe X-ray.
-
However, the appearance is consistent with normal early healing with inflammation or a superficial localized infection. Your dentist already said no dry socket; that’s reassuring — dry socket usually causes severe throbbing pain starting 2–4 days after extraction and an empty-looking socket with exposed bone.
Typical healing timeline (general)
-
First 24–72 hours: Clot forms, inflammation and some bleeding or oozing possible. Pain highest in this window.
-
3–7 days: Swelling and intense pain usually decrease. Granulation tissue begins to fill the socket.
-
7–14 days: Soft tissue (gum) starts covering the socket; pain should be minimal or gone.
-
2–3 weeks: Most of the socket surface epithelializes (closed over); chewing on that side often possible without problems.
-
6–12 weeks: Deeper healing and bone fill continue; full remodeling over months.
Your dentist’s “can take 3 weeks to start healing over” fits the normal range. If things are improving day-to-day, that’s a good sign.
If healing still ongoing at 14 days (what could happen / what to watch for)
Possible issues that can scale up if healing stalls:
-
Localized infection / abscess — increased pain, pus, bad taste/odor, swelling.
-
Delayed socket epithelialization (slow closure) — more risk of irritation and infection.
-
Alveolar osteitis (dry socket) — severe pain, foul taste, exposed bone (usually earlier, 2–5 days).
-
Spread of infection (rare if treated early) to adjacent tissue or spaces — causes visible swelling, fever, difficulty swallowing or breathing (urgent).
-
Medication-related problems (if on antibiotics for ear, they might not fully cover oral bacteria).
Practical, step-by-step plan (now → travel → if symptoms worsen)
Immediate care (do this now)
-
Hydrate and rest. Avoid heavy physical activity for 48 hrs.
-
Salt-water rinses: after the first 24 hrs, rinse gently with warm saline (1/2 teaspoon salt in 240 ml / 8 oz water) 4–6 times daily, especially after meals. Don’t rinse vigorously.
-
Oral hygiene: brush other teeth normally; be gentle around the extraction site. Don’t poke or pick the socket.
-
Pain control: use NSAIDs (ibuprofen 400–600 mg every 6–8 hrs as needed, unless contraindicated) and/or paracetamol. Follow dosing on the package or your doctor’s advice. Combining ibuprofen + paracetamol (staggered) is effective for dental pain.
-
Avoid: smoking, alcohol, hard/crunchy foods, straws, and sucking motions — these can dislodge clots or delay healing.
-
Soft diet: soups (not piping hot), yogurt, mashed potatoes, eggs, smoothies (no straw).
-
Continue prescribed meds your doctor gave unless a provider told you to stop. Note: antibiotics for your ear may or may not fully treat a dental infection. Don’t rely on them as definitive dental treatment unless your dentist specifically prescribed for oral infection.
If you travel Monday (short checklist)
-
If your pain is mild or improving, and you have no fever, spreading swelling, or uncontrolled pain, travel is usually OK with precautions: bring extra pain meds, saline rinse instructions, a copy/photo of dental note, and a plan for local dental care at destination.
-
If you have increasing pain, swelling, fever, pus, difficulty opening jaw, swallowing or breathing, do not travel — seek urgent dental/medical care and postpone travel if possible.
-
Take a clear photo of the site each day so you can show a dentist if needed.
If symptoms worsen or don’t improve by day 7–10
-
Return to your dentist or visit an emergency dental clinic. They may: examine, take an X-ray, prescribe a targeted antibiotic, perform local socket cleaning or place a medicated dressing, or drain an abscess if present.
Red flags — seek urgent care / emergency department now
-
Fever over 38°C (100.4°F) with worsening oral symptoms.
-
Rapidly increasing facial swelling or spreading to neck/eye area.
-
Difficulty breathing or swallowing.
-
Severe uncontrolled pain despite recommended analgesics.
-
Heavy or continuous bleeding that won’t stop after gentle pressure for 20–30 minutes.
What you should pack for travel / carry with you
-
Prescription/OTC pain meds (ibuprofen, paracetamol).
-
Written instructions from your dentist (or a photo of the extraction site and your dentist’s note).
-
Saline rinse instructions.
-
Contact info for nearest dental clinics at destination (use your directory: https://cebudentalimplants.com/map-dental-clinic or search for “emergency dentist” in the holiday area).
-
Any antibiotics you were prescribed and clear info on dosage.
Final thoughts / recommendation
-
Right now, from what you describe and the photo, this may be normal early healing. Your dentist’s reassurance that there’s no dry socket is helpful.
-
Still, don’t ignore worsening pain, fever, spreading swelling, or pus. If you notice any red-flag signs, get urgent care and postpone travel if needed.
-
If you want, I can:
-
Draft a one-page “dental status” note you can show at the clinic or carry while traveling (includes photo, symptoms, dentist’s quoted line), or
-
Help you prepare a checklist and find emergency clinics in the area you’re traveling to — but I’ll need the destination city (I can’t search the web from here).
-